
Designing for diversity: Dynamic persuasive strategies
in mHealth app development
⋆
Aleise H. McGowan
1,*,†
, Scott Sittig
2,∗,†
, Ryan Benton
3,†
, David Bourrie
3,†
, Sriram
Iyengar
4, †
and Aysu Dalogullari
1
1
The University of Southern Mississippi, Hattiesburg MS 39429, USA
2
University of Louisiana at Lafayette, Lafayette LA 70504, USA
3
University of South Alabama, Mobile AL 36688, USA
4
The University of Arizona, Tucson, AZ 85721, USA
Abstract
This study examines the impact of persuasive system design (PSD) in mobile health (mHealth) apps,
focusing on how personalized persuasive strategies, based on users’ psychological characteristics can
enhance engagement, behavior change and efficacy. With the ubiquity of mobile devices reshaping
behavior and perspectives, there's a growing need to personalize digital health technologies to
individual users’ characteristics. This approach challenges the conventional 'one size fits all' model,
recognizing the diversity in user needs and motivations. This research employed a multiphase
experimental design, developing and evaluating 25 mHealth app screens using PSD principles. This
involved rigorous prototyping, expert review, and iterative design, ensuring that each screen
effectively incorporated persuasive elements tailored for diverse user groups. The study's findings
highlight the effectiveness of combining primary task support and dialogue support in mHealth
screens to maximize user engagement. Furthermore, the research underscores the importance of
system credibility and social support in persuasive design, although these elements require careful
implementation due to users’ varying perceptions of persuasiveness among users. This work
significantly contributes to the field by providing insights into how digital health technologies can
be optimally designed to cater to the dynamic psychological makeup of users, ultimately enhancing
user engagement with a focus on behavior change.
Keywords
Persuasive Design, User Engagement, User-Centric Design, Digital Health Interventions 1
1. Introduction
The evolution of Behavior Change Systems (BCS) reflects a dynamic journey, from early
behaviorism ideas to the modern combination of psychology, data science, and user-centric
design, revealing a remarkable story of adaptation and creativity. The potential of BCS to
motivate and support individuals is promising; however, there needs to be more explicit
research on behavioral theory and evidence-based solutions [1]. Mobile health (mHealth) apps
have proven highly effective in encouraging positive health-related behavioral changes among
users [2]. Notably, the persuasive system design framework (PSD) plays a crucial role in guiding
BCSS 2024: The 12
th
International Workshop on Behavior Change Support Systems, April 10, 2024, Wollongong,
Australia.
∗
Corresponding author.
†
These authors contributed equally.
aleise.mcgowan@usm.edu (A. McGowan); scott.sittig@louisiana.edu (S. Sittig)
© 2024 Copyright for this paper by its authors. Use permitted under Creative Commons License Attribution 4.0 International (CC BY 4.0).
CEUR
Workshop
Proceedings
ceur-ws.org
ISSN 1613-0073
the use of persuasive technology, especially in mobile health applications [3, 4]. Recently,
mHealth interventions have gained interest as an innovative strategy to combat disease in a
cost-effective manner [5]. Regular evaluation of persuasive features within these mHealth apps
is essential, and the PSD model serves as a valuable tool for accomplishing this task. The benefits
of persuasive technologies in mHealth engagement, capable of educating, convincing, and
encouraging users throughout their behavioral change, particular in health behavior, are
significant and should not be overlooked [2]. The ubiquity of mobile devices has reshaped our
actions and thoughts, making it valuable and relevant for us to learn and understand the
importance of persuasive technology [6]. The word persuasive refers to synonyms like effective,
cueing, convincing, and compelling. At its root, persuasion is simply an attempt to influence
and convince others on various subjects [7].
Given the diverse range of individuals and their unique needs, the "one size fits all" approach
to solutions has been accepted as often counterproductive and outdated. Individuals vary
significantly in their needs, reflecting the diversity and uniqueness of their personal
characteristics and backgrounds [8]. It is important to accommodate cultural differences,
including race, gender, socioeconomic status, age, and sex, instead of applying one-size-fits-all
solutions in an effort to foster behavior change [9]. By embracing diversity and understanding
individual differences, we can achieve better outcomes, increased efficiency in innovation [10],
and better satisfaction [8]. Examining how individual psychological traits like self-efficacy,
health consciousness, and personality types influence user engagement with mHealth screens
highlights the importance of personalized digital health strategies [11].
2. Background
Digital health behavior change interventions have emerged as potent catalysts for positive
behavioral shifts among healthcare professionals, patients, and the public [12]. Mobile health
applications are evolving, with an increasing implementation of persuasive design features
aimed at enhancing behavior change [2]. A wide array of ideas, concepts, and approaches
comprises the behavior change interventions. These include, but are not limited to, the theory
of reasoned action, the theory of planned behavior, the technology of acceptance model, the
self-efficacy theory, the social cognitive theory, the elaboration likelihood model, cognitive
dissonance theory, goal setting theory, and computer self-efficacy [4]. In addition, the majority
of theories on cognitive health outline the possible connections between psychosocial elements
and healthful conduct [13]. Mobile applications target various health behaviors, including
increasing physical activity, smoking cessation, healthy eating, weight loss, and blood pressure
control, among others [14].
A systematic review of controlled trials in mobile health interventions revealed noteworthy
outcomes for therapies delivered via smartphones and tablets [15]. The findings indicate that
intervention participants demonstrated a heightened success rate in changes across a spectrum
of health behaviors and related outcomes. However, the implementation of mobile health
interventions faces significant challenges, such as user engagement, theoretical underpinnings,
pace and efficiency, effectiveness evaluation, regulation, and ethics. To address these problems
and maximize possibilities, a diverse range of academic disciplines, involving behavioral,
computer, and engineering sciences, as well as user-centered design, will need to collaborate
and share their skills [12]. Integrating behavior change interventions into mobile and social
technologies enables real-time, continuous evaluation, offering advantages over outdated, data-
poor, and infrequent methods.
A recent study focusing on computational models of habit formation proposed a method in
health applications for situations where actions are repeated continually; in promoting healthy
lifestyles, one of the obstacles to effective transformation is the process of breaking poor old
habits and developing healthy new ones [16].Previous research and development in persuasive
technology often adapted a one-size-fits-all approach [17]. Considering that individuals have
different motivations and beliefs, there is a need for digital health technology to become more
personalized [10]. In this literature review, we aim to explore the concept of personalization,
understanding diversity across different industries, and the importance of finding solutions that
are tailored to personal needs. One size does not fit all, especially when tailoring Persuasive
Technology (PT) to an individual [9]. Since persuasive systems aim to target behavior and shape
it into a desired behavior [18], understanding individual needs and adapting to various user
characteristics is essential.
Psychologically, consumer engagement improves when a mHealth app aligns with
individual user preferences, sparking interest and fostering sustained interaction and
commitment. This view, as discussed by Tarute et al., emphasizes how the consumers' focus is
drawn to brands or enterprises that resonate with their interests, thereby encouraging
cognitive, emotional, and behavioral engagement [19]. This includes maintaining commitment
and taking corresponding actions. Notably mHealth apps predominantly attract young adults,
with older adults showing less interest. This demographic skew, highlighted by Mustafa et al.
and Askari et al., narrows the consumer age range, since the elderly often show resistance to
adopting health apps [20, 21]. A significant challenge for mHealth apps lies in sustaining or
even initiating consumer interest. Factors contributing to this issue include missing elements
within the apps, lack of enjoyment, confusion regarding usage, and the need to evaluate
multiple apps to find the most effective ones [21].
There exists a paradigm shift in literature where researchers extended the qualifications for
engagement. Researchers began to home in on the principle of user engagement being driven
by the quality of the users/patients experience [22-24]. While others also measured engagement
by the interaction with digital health technologies, often driven by attributes that naturally
evoke interest in the consumer, which was frequently believed to be reflected by behavior
change in the user [25, 26]. Engagement is also seen as a synergized relationship between digital
health technology and the consumer, in which the consumer is fully immersed and aligned with
the activity [27].
User engagement is also driven by user characteristics. For example, emotional (i.e.
motivation) and behavioral (i.e. response to rewards) characteristics are considered driving
factors for the time and energy users are willing to expend [28]. Breaking from previous more
experience-oriented perspectives of engagement, current engagement concepts require the
users to give their undivided attention to the digital health technology [25]. Achieving synergy
between digital health technologies and consumers is often considered the highest form of user
engagement [27]. As smartphones and other conduits for the delivery of digital health
technologies become more ubiquitous, designers are capable of incorporating customization
features to engage users/patients [24].
While the positive influence that persuasion has on changing an individual's attitude and
behavior has been established [29, 30], researchers have contended the need for personalized
systems that address the individual's personality to increase the effectiveness of digital health
technologies [31, 32]. One-size-fits-all digital health technologies that target behavioral change
to improve the user's health often fail because they do not target the psychological traits that
drive an individual’s motivations and behaviors, due in part to the lack of guidance intervention
designers and data scientists with numerous options face [8].
A dynamic personalized approach to the development of persuasive technologies is
imperative as research has shown that strategies that may influence change in an individual
with one type of psychological type may dissuade another individual with a different
psychological type [9]. Our review of the literature revealed a void in the literature with
scientists seeking a more intimate view of the consumer and how they interact with persuasive
principles in order to help guide the design processes. The design process is furthered impaired
by the lack of an understanding of the psychological characteristics of digital health technology
users [33].
The common use of ‘Argumentum Ad Populum’ (“appeal to the majority”) in persuasive
technology becomes less effective over time as it fails to address the dynamic characteristics of
mHealth app users [34, 35]. Persuasive technology features become obsolete over time because
designers do not address the multivariate, dynamic characteristics of mHealth app users [36].
Given the flawed nature of the design process, to leverage the benefits of successfully engaging
the users of digital health technologies, it is desirable that dynamic features driven by user
characteristics are amalgamated into the design process to better serve the context of user
engagement [37, 38]. A methodical approach which intersects dynamic data driven design
facilitated by persuasive technology will allow researchers and designers of persuasive
technologies to predict the persuasive features that will successfully engage users, thus enabling
effective engagement. The following research study aims to address the challenge of designing
persuasive technology-grounded mHealth app screens that reflect the intended persuasive
characteristics of the designer.
With increasing application of user engagement in digital health technologies, the benefits
of enhanced outcomes are increasingly informed by mixed method approaches driven by data
science [39]. The integration of data science and psychological characteristics has led to
significant advances in predicting individual differences and similarities [40]. The use of data
science allows a user’s personality to be leveraged to anticipate his or her potential needs [41].
Contrast mining can identify the significant personality characteristic differences that may lead
to enhanced persuasiveness among groups of users and patients. By using this information,
designers of digital health technologies can establish enhanced guidelines for the
conceptualization of personalized persuasive intervention design for a given group; this, in turn,
would lead to improved engagement of users. The recognition of additional differences will in
turn allow designers of digital health technologies to better engage users and establish
guidelines in each user/patient group which would help in the conceptualization of a
personalized persuasive intervention design.
3. Methodology
3.1. Design process
To identify factors influencing engagement and intent to use a mHealth application, a multiple-
phase experiment was conducted during the Summer 2020. This experiment utilized a survey-
based approach, examining 25 mHealth app screens designed with persuasive principles to
promote physical activity. This study was conducted with the approval of the Institutional
Review Board (IRB) at the University of South Alabama, ensuring adherence to ethical standards
for research involving human participants. This research focuses on the design and validation
of the mHealth app screens. These screens were designed by adhering to the Persuasive System
Design (PSD) categories and principles delineated by Oinas-Kukkonen and Harjumaa [42]. The
screens were all developed with a unifying theme focused on enhancing and promoting physical
exercise. Contrast Mining was used to evaluate the screens, identifying significant differences
in user responses based on the interrelationships of the combinations of persuasive principles
and individual characteristics of the users [43]. Contrast mining is a subarea of data mining that
focuses on finding contrasting patterns that express significant differences in multiple datasets
or classes, often comparing cases with a desired outcome against those with an undesired
outcome [44].
The development process started with creating wireframe prototypes [45] for the mHealth
screens. In this phase, preliminary designs were sketched on paper, with each sheet serving as
a canvas for one mHealth app screen. Each prototype was thoroughly documented.
Documentation included the persuasive system category, the (primary) design principle as from
Oinas-Kukkonen's framework [42], targeted implantation, details about the mockup, and the
mockup name that would be used throughout the study. Table 1 shows an example of the initial
prototype development. Accompanying this documentation was a detailed description of each
screen's features, which was used to guide the assignment of a unique reference name for each
screen. This name was consistently used throughout the phases of questionnaire development
and subsequent analysis. The final step in this phase was the creation of a sketch for each
prototype, ensuring a visual representation of what each mHealth screen would encompass.
In the final development phase, BuildFire [46], a mobile application development tool was
used. Buildfire was used to create digital, high-fidelity prototypes for each mHealth app screen.
These advanced prototypes were instrumental in actualizing the design objectives set forth
during the wireframe stage. After development, still images of the mHealth screens were
captured using an iPhone XS Max. This technique was chosen to ensure that the captured
images would authentically represent the user's experience on a mobile device. The images
were then transferred from the iPhone to a laptop via email, for further analysis.
Table 1
Examples of the Initial Prototype Development Steps
Persuasive
System
Category
Design
Principle
Targeted
Implementation
Mockup Mockup
Name
Primary
Task
Support
Tunneling Guiding people in
a process step-by-
step to meet a
goal
Fitness program with
step by step workout
plan. Once daily/weekly
goals are reached, the
next set of steps are
given.
Burpee-
Squat

System
Credibility
Support
Trustworthiness Application
should appear to
be truthful, fair,
and unbiased
Display information
guaranteeing HIPAA
compliance to reassure
users that information
will not be shared with
3rd party organizations.
HIPAA
3.2. mHealth screen validation
In the final stage of the development process, the mHealth screen prototypes underwent a
rigorous evaluation by two distinguished experts in persuasive technology. This evaluation
used a blind review format for objective and unbiased assessment. The expert panel included
one reviewer with an extensive 12-year background in the field of persuasive technology and
another with 9 years of experience.
Following the expert inspection and blind review, a consultation was held with the expert
review panel where notes and suggestions were reviewed. The review and modification process
continued until the developer and reviewers reached a consensus. The mHealth screens were
iteratively evaluated, modified, and improved following each expert inspection and blind
review.
For the first round, twenty-three mHealth screens were developed: Add, Start, Burpee-Squat,
Increase, Mountain, Target, Trophy, Late, Calories, Dinner Chat, Tracker, About Us, Stories,
Leaderboard, Journal, Partners, Ads, Strategy, CDC, HIPAA, Contact, Before After, and Yoga.
The developer and reviewers identified eleven mHealth screens with conflicting persuasive
technology principles that required modification: Target, Dinner Chat, About Us, Journal,
Partners, Strategy, HIPAA, Contact, Before After, Yoga, and CDC. There were discrepancies in
the intended persuasive technology principle and the identified principle which necessitated
modifications in the mHealth app screen to ensure coherence in the application of persuasive
principles. The revised mHealth screens were resubmitted for review. CDC was dropped during
the first round because the designed persuasive category was not seen by either of the two
reviewers and the category that was identified was seen in another screen.
The Apple mHealth screen was created to replace CDC and submitted with revisions for
round 2. A consensus was reached on the twenty-three mHealth screens during the second
round. Additionally, three paper and high-fidelity prototypes were created for the remaining
persuasive technology principles following the methods stated above. The additional mHealth
screens (SSL, Avatar, and Recreation) were iteratively evaluated, modified, and improved using
expert inspection and blind review methods used during rounds one and two. The iterative
process resulted in twenty-five mHealth screens designed for the questionnaire that were
agreed upon through the blind review process and one mHealth screen prototype being
discarded. The mHealth screen acceptance by round is shown in Table 2. The X indicates which
round the mHealth screen was accepted and N/A indicates that the screen had not been
developed during the particular round.

Table 2
mHealth Screen Acceptance by Round
4. Results
The iterative process yielded twenty-five mHealth screens used in a comprehensive research
questionnaire.
Table 3 presents the final testing iteration, detailing the principles and principle categories
(PT = primary task support, DS = dialogue support, SC = system credibility support and SS =
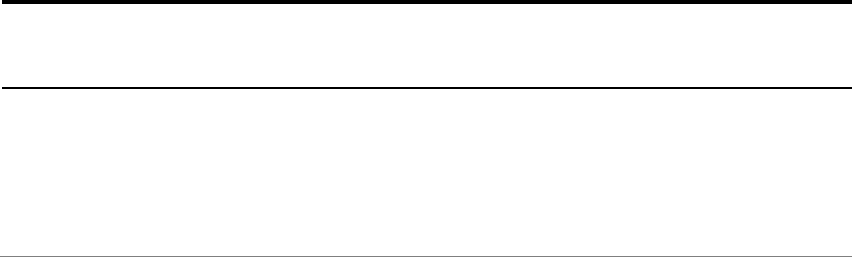
social support) for each screen. Figure 1 displays two of the final mHealth screens (Start and
Contact) that were developed.
Screen Name Round 1 Round 2 Round 3
Add X
Start X
Burpee-Squat X
Increase X
Mountain X
Target X
Trophy X
Late X
Calories X
Dinner Chat X
Tracker X
About Us X
Stories X
Leaderboard X
Journal X
Partners X
Ads X
Strategy X
Cdc Dropped N/A N/A
Hipaa X
Contact X
Before After X
Yoga X
Apple N/A Replaced Cdc
Ssl N/A N/A X
Avatar N/A N/A X
Recreation N/A N/A X

Table 3
Mobile App Screen Name with Persuasive principles and Categories
Screen Name Principle 1 (Primary) Principle 2 Principle 3
Add (PT) Tailoring (PT) Tunneling
Start (PT) Reduction (PT) Tunneling
Burpee-Squat (PT) Tunneling (PT) Reduction
Increase (DS) Praise
Mountain (PT) Rehearsal (DS) Suggestion
Target (DS) Praise (PT) Personalization
Trophy (DS) Rewards (DS) Praise
Late (DS) Reminders
Calories (DS) Suggestion
Dinner Chat (DS) Social Role (DS) Praise
Tracker (PT) Self-Monitoring
About Us (SC) Expertise (SC)Trustworthiness (SC) Authority
Stories (SS) Recognition (PT) Simulation (DS) Praise
Leaderboard (SS) Competition
Journal (SS) Social Learning (SS) Social Comparison (SC)Social
Facilitation
Partners (SC) Trustworthiness (SC) Expertise (SC) Authority
Ads (SC) Surface Credibility
Strategy (SC) Authority (SC) Expertise
Apple (SC) Verifiability (SC) Expertise (SC) Authority
HIPAA (SC) Trustworthiness (SC) Surface Credibility
Contact (SC) Real-World Feel
Before After (SC) Normative Influence (PT) Simulation
Yoga (SS) Cooperation (DS) Praise (SS)Social
Comparison
SSL (SC)Third-party
Endorsements
(SC) Trustworthiness
Avatar (DS) Similarity (DS) Liking
Figure 1: Sample mHealth screens developed and accepted during review
Among the 25 screens developed, 5 (20%) featured a primary principle from the primary task
support category, 7 (28%) from the dialogue support category, 8 (32%) from the system
credibility support category, and 5 (20%) from the social support category.
Contrast mining, not driven by hypothesis, effectively uncovers strong correlations between
predictors, guiding future research. This method produced a concise set of rules predicting the
persuasiveness of mHealth screens’ primary categories: primary task support, dialogue support,
system credibility support, or social support would be persuasive. The primary task support
scores exceeded the average perceived persuasiveness score, with screens from the system
credibility category closely matching or surpassing the average score.
This study introduces contrast mining as a novel solution to the gap in PSD frameworks’
lack of systematic data driven decisions. Contrast mining offered a multi-layer insight into its
impact on perceived persuasiveness at the screen level. The Primary Task Support category
ranked highest in the weighted perceived persuasiveness bin. This finding contradicts Drozd
[47], who found no significant relationship between primary task support and perceived
persuasiveness. Screens from the System Credibility category achieved mid-level weighted
perceived persuasiveness scores. The findings that primary task support and system credibility
increase perceived persuasiveness are supported by Lehto [48], who found that primary task
support and system credibility both significantly impact perceived persuasiveness directly.
Screens from the Social Support category scored in the lowest perceived persuasiveness bin.
Figure 2 illustrates the bins of perceived persuasiveness rules generated by Contrast Mining.
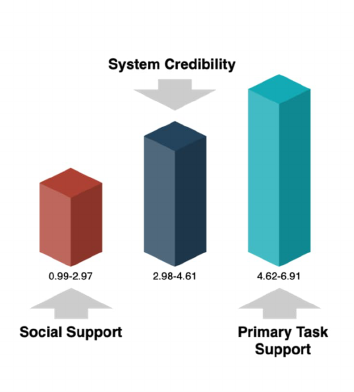
Figure 2: Contrast mining category results
The findings suggest that practitioners seeking to develop persuasive digital health
technologies should develop screens using techniques in the primary task support or system
credibility categories. Screens that employ techniques from the social support category need to
be “strongly personalized” in order to achieve perceived persuasive-ness as these produced low
perceived persuasiveness scores in our study. The contrast mining findings also suggest
practitioners should use techniques from the dialogue support category when developing digital
health technologies.
Little is known about the impact of psychological characteristics and the combination of
multiple persuasive techniques on perceived persuasiveness. Drozd et al. [47] discovered that
Primary Task Support and Dialogue Support together significantly impacted perceived
persuasiveness. Additional studies that examine the primary and secondary categories are
needed to determine whether or not the combination of additional categories is driving the
perceived persuasiveness.
5. Discussion
Incorporating accurate persuasive design principles into a mHealth design process involves a
detailed and multifaceted approach [42]. This strategy involves seamlessly blending these
principles into the user experience of the digital health technology.
The Primary Task Support category plays a crucial role in simplifying the user's journey by
breaking down complex tasks into simpler, more manageable steps. This was achieved through
the reduction principle (Start), which simplified the steps involved in starting the weight loss
journey, and the tunneling method (Burpee Squat), which guided users step-by-step in the
process of completing an exercise. The design also incorporated tailoring (Add), adapting the
app’s interface and functionality to individual user needs, interests, and personalities, creating
a more customized experience. To enhance engagement and motivation, personalization
(Target) was a key focus, ensuring that users received timely suggestions, praise, and rewards.
Additionally, self-monitoring (Tracker) features were integrated, allowing users to easily track
their progress and performance. The app also included simulation (Before After) and rehearsal
(Mountain), which depicted a video with a coach showing users how to properly perform an
exercise.
Similarly, the Dialogue Support category enriches the interaction between humans and
digital health technologies, rendering the application more captivating and reactive. This
included integrating aspects like praise and rewards (Increase, Trophy), with the app providing
various forms of positive feedback and visual rewards for task completion and reaching health
milestones. In addition, the app included reminders (Late) and tailored suggestions (Calories),
where reminders helped users stay on track with their health goals and personalized
suggestions offered advice based on individual user data. The design also focused on the
principles of similarity (Avatar) and liking (Avatar), ensuring that the app was not only visually
appealing but also relatable to the users.
The System Credibility category aims to build trust and reliability within the system.
Achieving this involved certifying the app’s trustworthiness (Partners), presenting it as honest
and unbiased to the user. To demonstrate expertise (About Us), the app included content from
knowledgeable and reputable health organizations. Surface credibility (Ads) was also a focus,
achieved through a competent and visually credible ad free design that resonated with users.
Additionally, the app provided a real-world feel (Contact) by connecting users with the
organizations and individuals responsible for the content, thereby enhancing the authenticity
of the information provided. Authority (Strategy) was leveraged by incorporating inputs from
recognized experts and authorities in the field such as the CDC and leading weight loss
authorities, thereby bolstering user trust. To further solidify credibility, the app included third-
party endorsements (SSL) and features for verifiability, allowing users to cross-check and
confirm the safety of their health data with external sources.
Finally, the Social Support category leverages social influence to motivate users. This is
accomplished through the social learning (Journal) principle, which allow users to see others
engaging in target behaviors, creating a sense of community and shared goals. Additionally, the
app incorporates social comparison (Journal) principle, enabling users to measure their
performance against that of their peers, which serves as a motivational tool. The use of
normative influence (Before After) is also employed, harnessing peer pressure in a positive way
to encourage desired behaviors, by sharing before and after pictures of users that lost more than
fifty pounds. Social facilitation (Journal) is integrated to give users the feeling of being part of
a collective effort by allowing them to participate alongside others. The mHealth app screens
also tapped into the innate human tendencies towards cooperation (Yoga) and competition
(Leaderboard), encouraging both collaborative and competitive activities which are designed to
increase engagement. Furthermore, the app includes features for recognition (Stories), publicly
acknowledging user achievements, which not only rewards but also motivates users to continue
their health journey.
Each of these categories and principles is interwoven into the design process to create a
persuasive, engaging, and effective digital health technology that resonates with users on
multiple levels, encouraging positive behavior change and sustained engagement.
6. Conclusion
This study aimed to investigate the effectiveness of persuasive design principles in mHealth
applications and how they contribute to user engagement and perceived persuasiveness. This
research advances the field of persuasive technology by focusing on the user-centric design and
validation of mHealth app screens, employing data-driven methods to assess their effectiveness
in engaging users and influencing behavior change. The use of dynamic data-driven capabilities
is important to advancing perceived persuasiveness which has the potential to successfully
engage users of digital health technologies. A significant limitation of this study was the use of
static screens. Developing a fully developed app will allow researchers to evaluate the
engagement of the digital health tool. Running these studies in tandem will allow researchers
to evaluate engagement on both of those to see if higher perceived persuasiveness leads to
higher engagement.
While this study has provided valuable insights into the application of persuasive design
principles in mHealth applications, further clarification is needed regarding the extent of
personalization in these designs. Understanding how various levels of personalization influence
user engagement and the effectiveness of persuasive strategies could significantly enhance the
development of more tailored and impactful digital health interventions. Future research in this
area should explore the nuances of personalization, examining its potential to meet diverse user
needs and preferences more effectively.
References
[1] A. C. King et al., "Effects of Three Motivationally Targeted Mobile Device Applications on
Initial Physical Activity and Sedentary Behavior Change in Midlife and Older Adults: A
Randomized Trial," PLoS One, 11(6): e0156370 (2016). doi: 10.1371/journal.pone.0156370.
[2] J. Matthews, K. T. Win, H. Oinas-Kukkonen, and M. Freeman, "Persuasive Technology in
Mobile Applications Promoting Physical Activity: a Systematic Review," J Med Syst, 40(3):
72 (2016). doi: 10.1007/s10916-015-0425-x.
[3] A. Hussian, A. Mateen, F. Amin, M. A. Abid, and S. Ullah, "Health Monitoring Apps: An
Evaluation of the Persuasive System Design Model for Human Wellbeing," Information,
14(7), (2023). doi: 10.3390/info14070412.
[4] H. Oinas-Kukkonen, "A foundation for the study of behavior change support systems,"
Personal and Ubiquitous Computing, 17(6): 1223-1235, (2012). doi: 10.1007/s00779-012-
0591-5.
[5] S. Sittig, A. McGowan, and S. Iyengar, "Extensive Review of Persuasive System Design
Categories and Principles: Behavioral Obesity Interventions," J Med Syst, 44(7): 128, (2020).
doi: 10.1007/s10916-020-01591-w.
[6] B. J. Fogg, "Creating Persuasive Technologies: An Eight-Step Design Process," presented at
the Proceedings of the 4th International Conference on Persuasive Technology - Persuasive
'09 (2009).
[7] H. A. A. Spelt, J. H. D. M. Westerink, L. Frank, J. Ham, and W. A. Ijsselsteijn, "Physiology-
based personalization of persuasive technology: a user modeling perspective," User
Modeling and User-Adapted Interaction (2022). doi: 10.1007/s11257-021-09313-8.
[8] E. Engl, P. Smittenaar, and S. K. Sgaier, "Identifying population segments for effective
intervention design and targeting using unsupervised machine learning: an end-to-end
guide," Gates Open Res, 3:1503, (2019), doi: 10.12688/gatesopenres.13029.2.
[9] A. M. Abdullahi, K. Oyibo, R. Orji, and A. A. Kawu, "The Influence of Age, Gender, and
Cognitive Ability on the Susceptibility to Persuasive Strategies," Information, 10(11),
(2019). doi: 10.3390/info10110352.
[10] R. Orji, "Exploring the persuasiveness of behavior change support strategies and possible
gender differences," presented at the 2nd International Workshop on Behavior Change
Support Systems, BCSS 2014, Padua; Italy, (2014).
[11] A. McGowan, S. Sittig, D. Bourrie, R. Benton, and S. Iyengar, "The Intersection of
Persuasive System Design and Personalization in Mobile Health: Statistical Evaluation," (in
English), JMIR Mhealth Uhealth, 10(9): e40576, (2022). doi: 10.2196/40576.
[12] S. Michie, L. Yardley, R. West, K. Patrick, and F. Greaves, "Developing and Evaluating
Digital Interventions to Promote Behavior Change in Health and Health Care:
Recommendations Resulting From an International Workshop," J Med Internet Res, 19(6):1-
13, (2017). doi: 10.2196/jmir.7126.
[13] F. Taj, M. C. A. Klein, and A. Van Halteren, "Motivating Machines: The Potential of
Modeling Motivation as MoA for Behavior Change Systems," Information, 13(5), (2022).
doi: 10.3390/info13050258.
[14] C. Ernsting et al., "Using Smartphones and Health Apps to Change and Manage Health
Behaviors: A Population-Based Survey," J Med Internet Res, 19(4):e101, (2017). doi:
10.2196/jmir.6838.
[15] W. T. Riley, D. E. Rivera, A. A. Atienza, W. Nilsen, S. M. Allison, and R. Mermelstein,
"Health behavior models in the age of mobile interventions: are our theories up to the
task?," Transl Behav Med, 1 (1):53-71, (2011). doi: 10.1007/s13142-011-0021-7.
[16] C. Zhang, J. Vanschoren, A. van Wissen, D. Lakens, B. de Ruyter, and I. J. WA, "Theory-
based habit modeling for enhancing behavior prediction in behavior change support
systems," User Model User-adapt Interact, 32(39):389-415, (2022). doi: 10.1007/s11257-022-
09326-x.
[17] A. M. Abdullahi, R. Orji, and A. A. Kawu, "Gender, Age and Subjective Well-Being:
Towards Personalized Persuasive Health Interventions," Information, 10(10), (2019), doi:
10.3390/info10100301.
[18] V. Mylonopoulou, "Design for health behavior change supportive technology," presented
at the Proceedings of the 10th Nordic Conference on Human-Computer Interaction -
NordiCHI '18, 2018.
[19] A. Tarute, S. Nikou, and R. Gatautis, "Mobile application driven consumer engagement,"
Telematics and Informatics, vol. 34, no. 4, pp. 145-156, 2017, doi: 10.1016/j.tele.2017.01.006.
[20] M. Askari, N. S. Klaver, T. J. van Gestel, and J. van de Klundert, "Intention to use Medical
Apps Among Older Adults in the Netherlands: Cross-Sectional Study," J Med Internet Res,
vol. 22, no. 9, p. e18080, Sep 4 2020, doi: 10.2196/18080.
[21] A. S. Mustafa, N. Ali, J. S. Dhillon, G. Alkawsi, and Y. Baashar, "User Engagement and
Abandonment of mHealth: A Cross-Sectional Survey," Healthcare (Basel), vol. 10, no. 2, Jan
24 2022, doi: 10.3390/healthcare10020221.
[22] S. Taki et al., "Assessing User Engagement of an mHealth Intervention: Development and
Implementation of the Growing Healthy App Engagement Index," JMIR Mhealth Uhealth,
vol. 5, no. 6, p. e89, Jun 29 2017, doi: 10.2196/mhealth.7236.
[23] M. Holdener, A. Gut, and A. Angerer, "Applicability of the User Engagement Scale to
Mobile Health: A Survey-Based Quantitative Study," JMIR Mhealth Uhealth, vol. 8, no. 1,
p. e13244, Jan 3 2020, doi: 10.2196/13244.
[24] M. Lalmas, H. O’Brien, and E. Yom-Tov, Measuring User Engagement (Synthesis Lectures
on Information Concepts, Retrieval, and Services). Morgan & Claypool, 2014.
[25] X. Ren, C. Silpasuwanchai, and J. Cahill, "Human-Engaged Computing: the future of
Human–Computer Interaction," CCF Transactions on Pervasive Computing and
Interaction, vol. 1, no. 1, pp. 47-68, 2019, doi: 10.1007/s42486-019-00007-0.
[26] N. Zagalo, "From Experience to Engagement," in Engagement Design: Designing for
Interaction Motivations. Cham: Springer International Publishing, 2020, pp. 11-30.
[27] K. Salehzadeh Niksirat et al., "Approaching Engagement towards Human-Engaged
Computing," presented at the Extended Abstracts of the 2018 CHI Conference on Human
Factors in Computing Systems, 2018.
[28] H. L. O'Brien, J. Arguello, and R. Capra, "An empirical study of interest, task complexity,
and search behaviour on user engagement," Information Processing & Management, vol.
57, no. 3, 2020, doi: 10.1016/j.ipm.2020.102226.
[29] P. MScMed and F. G. BOccTher, "Persuasive technology and behaviour change in parent-
focused eHealth interventions supporting child health: A scoping review protocol," New
Zealand Journal of Physiotherapy, 47(1): 36-48 (2019).
[30] R. Orji and K. Moffatt, "Persuasive technology for health and wellness: State-of-the-art and
emerging trends," Health Informatics J, 24(1):66-91 (2018). doi: 10.1177/1460458216650979.
[31] M. Kaptein, P. Markopoulos, B. de Ruyter, and E. Aarts, "Personalizing persuasive
technologies: Explicit and implicit personalization using persuasion profiles," International
Journal of Human-Computer Studies, vol. 77, pp. 38-51, 2015, doi:
10.1016/j.ijhcs.2015.01.004.
[32] H. J. Wall, C. C. Campbell, L. K. Kaye, A. Levy, and N. Bhullar, "Personality profiles and
persuasion: An exploratory study investigating the role of the Big-5, Type D personality
and the Dark Triad on susceptibility to persuasion," Personality and Individual Differences,
139:69-76, (2019). doi: 10.1016/j.paid.2018.11.003.
[33] M. Tuman and A. Moyer, "Health intentions and behaviors of health app owners: a cross-
sectional study," Psychol Health Med, 24(7):819-826, (2019). doi:
10.1080/13548506.2019.1576911.
[34] E. Anagnostopoulou, E. Bothos, B. Magoutas, J. Schrammel, and G. Mentzas, "Persuasive
technologies for sustainable mobility: State of the art and emerging trends," Sustainability,
10(7):2128, (2018).
[35] R. Orji and R. L. Mandryk, "Developing culturally relevant design guidelines for
encouraging healthy eating behavior," International Journal of Human-Computer Studies,
72(2):207-223, (2014).
[36] H. Oinas-Kukkonen, "Personalization Myopia: A Viewpoint to True Personalization of
Information Systems," presented at the Proceedings of the 22nd International Academic
Mindtrek Conference on - Mindtrek '18, (2018).
[37] J. A. Naslund et al., "Health behavior models for informing digital technology interventions
for individuals with mental illness," Psychiatr Rehabil J, 40(3):325-335, (2017). doi:
10.1037/prj0000246.
[38] D. Spruijt-Metz and W. Nilsen. (2014, July-Sept. 2014) Dynamic Models of Behavior for
Just-in-Time Adaptive Interventions. IEEE Pervasive Computing 13-17.
[39] R. K. Britt, J. Maddox, S. Kanthawala, and J. L. Hayes, "The impact of mHealth
interventions," in Technology and Health, pp. 271-288, (2020).
[40] W. Bleidorn and C. J. Hopwood, "Using Machine Learning to Advance Personality
Assessment and Theory," Pers Soc Psychol Rev, 23(2):190-203, (2019). doi:
10.1177/1088868318772990.
[41] A. Souri, S. Hosseinpour, and A. M. Rahmani, "Personality classification based on profiles
of social networks’ users and the five-factor model of personality," Human-centric
Computing and Information Sciences, 8(1), (2018). doi: 10.1186/s13673-018-0147-4.
[42] H. Oinas-Kukkonen and M. Harjumaa, "Persuasive Systems Design: Key Issues, Process
Model, and System Features," Communications of the Association for Information Systems,
24, (2009). doi: 10.17705/1cais.02428.
[43] Contrast. (2018). GitHub. Accessed: 08/13/2021. [Online]. Available:
https://github.com/parsahosseini/contrast
[44] G. Dong and J. Bailey, Contrast data mining: concepts, algorithms, and applications. CRC
Press, (2012).
[45] E. Rosenzweig, Successful user experience : strategies and roadmaps. Amsterdam: Elsevier,
(2015).
[46] Buildfire Corporation. https://buildfire.com/
[47] F. Drozd, T. Lehto, and H. Oinas-Kukkonen, "Exploring Perceived Persuasiveness of a
Behavior Change Support System: A Structural Model," in Persuasive Technology. Design
for Health and Safety, (Lecture Notes in Computer Science, ch. 14, pp. 157-168, (2012).
[48] T. Lehto, H. Oinas-Kukkonen, and F. Drozd, "Factors affecting perceived persuasiveness of
a behavior change support system," (2012).
